You’re probably familiar with the human genome, and its 20,000 genes that form the blueprint for our bodies. These genes are crucial, but they aren’t on the frontlines of biology. Rather, they provide instructions for making the proteins that give shape to our cells, facilitate chemical reactions, and generally keep life running smoothly.
Collectively, the set of all proteins found in a cell, tissue, or sample is known as the proteome. The study of this elaborate cast of characters and their myriad interactions is called proteomics. As World Health Day (April 7) draws near, it’s worth reflecting on the importance of proteins in the body in keeping us well. Dig down to the root of many diseases, and you’ll often find a malfunctioning or missing protein.
With help from emerging proteomics technologies, like the Nautilus Proteome Analysis Platform, researchers are poised to unlock protein-based insights that could lead to improved health outcomes for millions of people around the world. In some cases, they already have. To illustrate the power of this knowledge, here are a few stories of hope and success, each centered on a specific ailment and its connection to proteins in the body.
This post is part of our series on the incredible power of proteins. For more from this series, check out our post on the Klotho protein’s ability to enhance cognition in aged monkeys and our post on FGF21’s ability to help mice sober up.
Watch this video for a brief intro to proteomics:
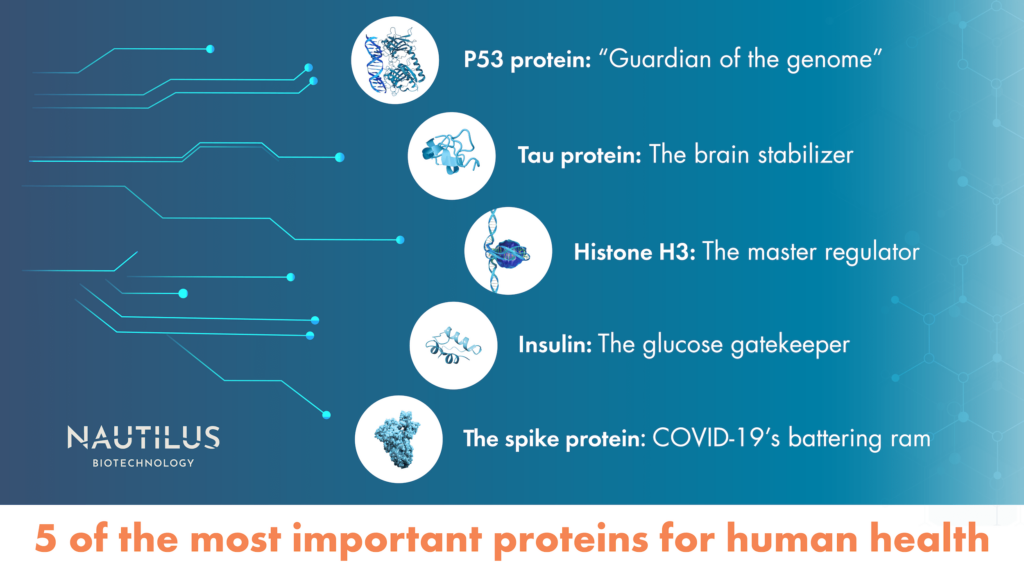
P53 protein: “Guardian of the Genome”
When cancer cells start multiplying out of control as a result of DNA damage, one of the most important proteins in the body is p53, which is made by the TP53 gene. The p53 protein halts cell division, buying time to repair the DNA or induce apoptosis, programmed cell death. Thanks to its knack for preventing tumor development, p53 has been dubbed the “guardian of the genome.” But when TP53 mutations prevent this protein from performing its duties, we’re far more prone to cancer — virtually all tumors involve some dysfunctional version of the p53 protein.
Recently, a few drugs targeting mutated forms of p53 have progressed to clinical trials. Some of the most promising cause mutated p53 to refold and essentially return to its normal, cancer-preventing form. One such drug, eprenetapopt, has completed a phase III clinical trial, though data on clinical efficacy is still needed.
Princeton molecular biologist Arnold Levine, writing in a paper published last year, notes that it took four decades of research on the p53 protein and other cancer-associated proteins “to understand the pathways they command, how they function, and how they interact with the environment of the cells they control.”
Now, with highly efficient tools for exploring the proteome, it will be easier than ever for scientists to design precision drugs for cancer that target p53 mutations and watch to see how they affect tumor growth. Rapid-throughput proteomics tools with easier workflows can be brought into the clinic, where doctors can use them to screen for mutated p53 proteins at earlier stages of cancer, and see exactly which mutations are there. With that knowledge, they can apply drugs targeted to those mutations, and watch to see how they work in almost real time.
Watch our animation to learn about applications of proteomics in cancer research:
Tau protein: The brain stabilizer
Many studies of Alzheimer’s disease focus on the tau protein. While the links tying this protein to the disease still aren’t crystal clear, we do know that Alzheimer’s is associated with dense tangles of tau protein in the brain.
In a healthy brain, tau proteins bind to microtubules, a structural component of neurons and other cells, but in Alzheimer’s disease the tau protein clumps together with other tau molecules in “neurofibrillary tangles” that may lead to cognitive degeneration. Potential treatments targeting tau proteins have recently gotten more attention from scientists, as the underlying biology of these tangles has become clearer.
Nevertheless, given that decades of research into the tau protein in Alzheimer’s haven’t yielded definitive answers, we may need to expand our search. In a 2020 paper in Neuropsychopharmacology Reviews, a group of neurologists suggests that a more systems-based proteomics approach might be required to understand how the tau protein is linked to the disease. Network proteomic analysis, which organizes data into modules of protein co-expression associated with different phenotypes, could be one answer, they suggest, offering a more holistic view that could finally unlock the tau protein puzzle.
Watch this animation to learn how the Nautilus Platform may enable researchers to learn more about proteoforms like the tau proteoforms in Alzheimers:
Histone H3: The master regulator
Epigenetics is a process by which behaviors and environment alter gene expression, or which genes are turned on or off at a given time.
For this, one of the most important class of proteins in the body involved in epigenetics is histones. These proteins act as spools that DNA winds around, creating structures called nucleosomes. One histone protein in particular, called histone H3, is thought to be particularly important for epigenetic control of gene expression.
H3 can be modified by processes like acetylation and methylation, which involve adding small molecules, called acetyl and methyl groups, respectively, to the protein, changing its structure and function. These new versions of the protein are called proteoforms. Histone modifications can in turn change how genes are expressed, or turned into functional proteins in the body.
H3 modifications are implicated in many diseases, including autoimmune diseases, neurodevelopmental conditions, and cancer. Drugs specifically targeting histones, including H3, are already in clinical trials, and could offer precise treatments for cancer and other diseases linked to gene expression.
Studying the numerous potential H3 proteoforms and their roles in disease will be a key part of creating epigentics-based precision medicines. Comprehensive proteomics platforms that can identify and compare multiple H3 proteoforms at once would provide a far more holistic view of this protein across cell types and states. That will make it easier for researchers to link these proteoforms to specific diseases, and design and test potential treatments.
Insulin: The glucose gatekeeper
Type 2 diabetes, a mounting epidemic that affects more than 10% of the global adult population, is triggered by the body’s resistance to insulin. Insulin is a protein that enables glucose to enter cells, where they convert it into fuel. But in patients with Type 2 diabetes, cells don’t respond normally to insulin, so all that glucose keeps circulating in the blood. Today, the drug metformin is a first-line treatment for Type 2 diabetes; it works by decreasing glucose production in the liver and sensitizing cells to insulin proteins in the body so they can take more glucose out of the bloodstream.
Even more powerful treatments could be on the horizon. In a 2020 paper in Circulation Research, two Harvard researchers write that large-scale protein analysis has “given us unprecedented insight” into early biomarkers for diabetes, potentially opening the door for screening, diagnosis, and prognosis a decade or more before its onset. Dozens of proteins have already been linked to insulin resistance and prediabetes, and future studies could illuminate the roles they play in the progression of diabetes.
The spike protein: COVID-19’s battering ram
Perhaps the greatest health breakthrough in recent years centers on a single protein: the so-called “spike protein” that the SARS-CoV-2 virus uses to penetrate human cells. Powered by the spike protein, SARS-CoV-2 has caused more than 700 million COVID cases and nearly 7 million deaths worldwide. The SARS-CoV-2 spike protein is unique, conspicuous and located on the surface of viral cells, making it a great target for vaccines, which teach the body to find and attack the spike protein with antibodies.
Though much of the world has attempted to return to normal, SARS-CoV-2 continues to infect more than a hundred thousand people every day, and new variants of the disease could emerge at any time. Proteomics, along with other “-omics” like genomics and transcriptomics could play an important role in quickly diagnosing Covid infections and classifying disease severity, a team of Chinese researchers wrote in a paper published in Virulence in May. In the event of severe outbreaks, proteomic analysis may even predict survival rates among patients and improve hospital triaging, helping to keep ICUs from overflowing as they did in the early days of the pandemic.
The future most important proteins
Proteins like tau, p53, and H3 are considered some of the most important in the world today because of what we know about how they impact human health, but much of the proteome remains hidden from view. By exploring still-mysterious regions of the proteome with next-generation proteomics tools, we may add new proteins to the list of the most important.
There could be proteins and proteoforms that carry out tasks currently unknown to us, or which play a far bigger role in life than we’d ever imagined. Only as we delve deeper into the proteome will we know for sure. Perhaps someone writing this same article in ten years will have a very different perspective on what’s important!
Watch our animation to learn how our the Nautilus Platform is designed to comprehensively quantify the proteome
MORE ARTICLES


