Proteomics is the study of all the proteins in a cell, sample, or organism. Proteins perform nearly all biological functions. Thus, a better understanding of the proteome may alter the way we do research, vastly improve drug development, and revolutionize precision medicine. One of the most exciting applications of proteomics is protein biomarker discovery.
What is protein biomarker discovery?
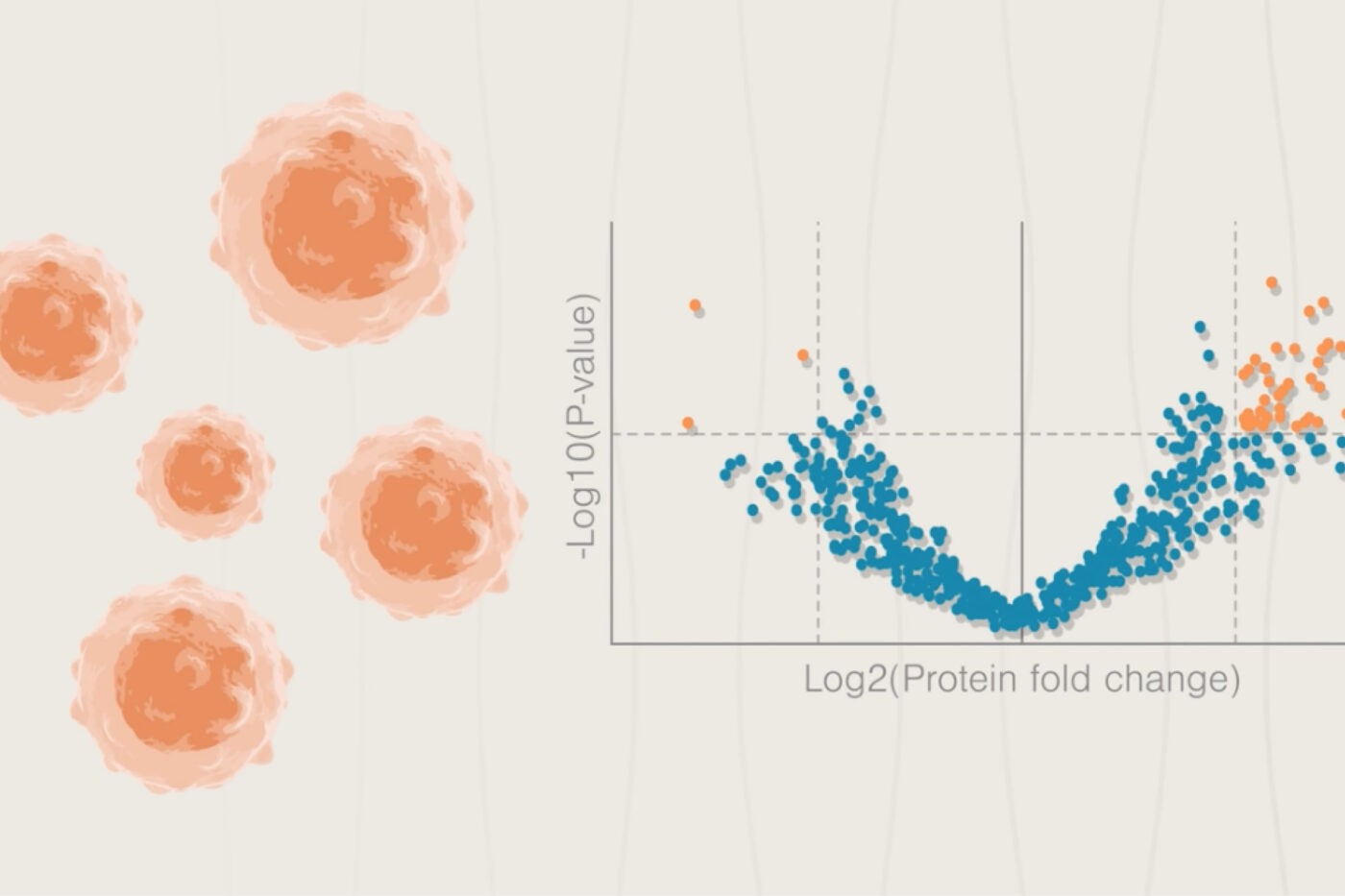
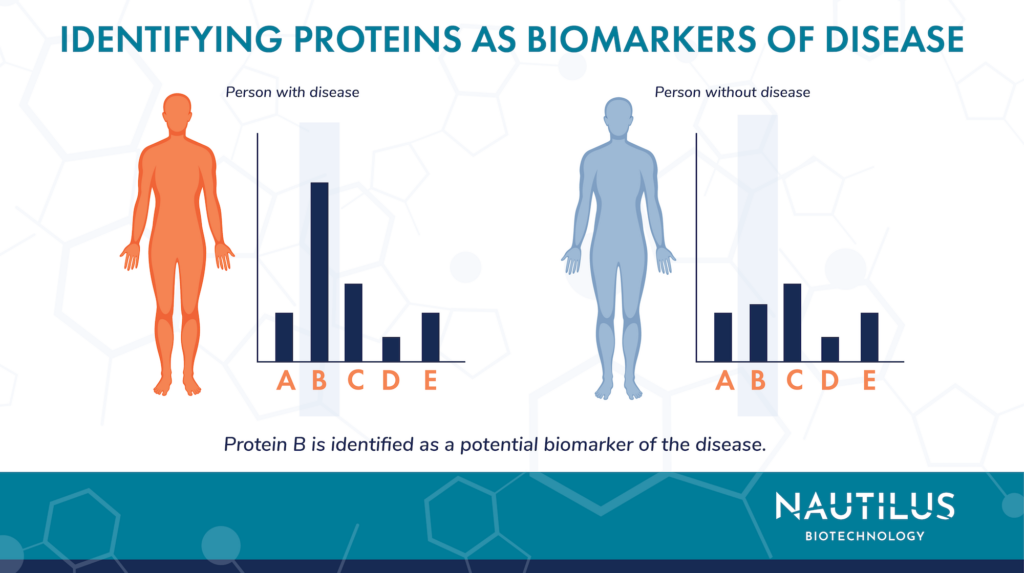
Biomarkers are biological signals that can be measured to assess normal and abnormal biological processes. Any proteins or patterns of protein expression that change in diseased cells may be good protein biomarkers. Discovering these protein biomarkers is an important goal of many scientific studies into diseases like cancer. Protein biomarker discovery involves identifying the proteins present in a sample — its proteome — and then using proteomic analysis to see which proteins are associated with a process of interest. For example, seeing that levels of Human Epidermal Growth Factor Receptor (HER2) are higher in samples from patients with aggressive breast cancer vs those with less aggressive breast cancer is an indication HER2 is a biomarker for breast cancer aggressiveness.
Researchers have already found proteomics biomarkers for tuberculosis, HIV, autoimmune diseases, cancer, and more. More research needs to be done to validate these biomarkers and apply them in the clinic, but these studies are establishing a strong evidence base for future work to build on.
Below we discuss a few disease areas where proteomics is already having an impact and where next generation proteomics technologies like the Nautilus Platform can potentially fill gaps in our set of clinical useful biomarkers. Researchers can potentially use these newfound biomarkers to create novel tests that enable doctors to better diagnose and treat diseases that impact millions of people.
Learn more about the intersection of proteomics and biomarkers in this episode of our Translating Proteomics podcast
Studying cancer biomarkers using proteomics
Scientists have identified cancer biomarkers for nearly every kind of tumor. Diagnoses using protein biomarkers could both speed up the process of diagnosis and point toward more precise treatments for specific cancers.
For example, most cases of ovarian cancer are currently diagnosed when the disease is already advanced, and survival odds are low. That’s in part because imaging potentially cancerous cells is difficult, and many ovarian tumors metastasize before they’re big enough to be seen.
While there are known protein biomarkers for the disease, the most common one, CA125, only positively identifies early cases of ovarian cancer about 50% of the time. Researchers are currently using proteomics to look for new ovarian cancer biomarkers that could catch the disease in its first stage, when the five year survival rate is over 90 percent.
Protein biomarkers could also help doctors distinguish ovarian and colon cancer, which are difficult to tell apart in earlier stages of disease. That would allow targeted treatments to happen earlier, potentially saving lives.
Autoimmune disease biomarkers: A prime proteomics application
Autoimmune diseases like multiple sclerosis, lupus, Crohn’s disease, and rheumatoid arthritis are characterized by proteins called autoantibodies that attack the body’s own tissues. Diagnosing autoimmune diseases remains challenging today because many of the most common symptoms, like swelling or pain, are non-specific.
Protein biomarkers could be far more specific. Each autoimmune disease likely has its own set of protein biomarkers that could be used for diagnosis. For example, current and future work may be able to pick out specific sets of autoantibodies for each autoimmune disease, which can be later validated as diagnostic biomarkers.
Toward similar ends, researchers recently published work in the Journal of Proteome Research where they used proteomics profiling to differentiate patients with four different autoimmune diseases — systemic lupus erythematosus, ANCA-associated systemic vasculitis, rheumatoid arthritis, and Sjögren’s syndrome. They successfully differentiated people with the diseases from one another as well as healthy controls.
With more comprehensive, next-generation proteomics platforms – like the Nautilus Proteome Analysis Platform – these studies may be easier to perform and validate in patients. This could make it possible to diagnose autoimmune diseases just by looking at a patient’s proteome.
Applying proteomics to biomarker discovery and beyond
Next-generation proteomics analysis platforms are expected to speed up the process of discovering protein biomarkers and may enable the development of diagnostic tools that vastly improve our ability to identify diseases in their early stages. Excitingly, biomarkers are just one of the many applications of proteomics in medicine. Analyzing changes to the proteome could help show whether treatments are working and help to personalize medicine. Other proteomic analyses might show how different pathogens infect the body or how tumors grow — and that’s just scratching the surface.
The field of proteomics is poised to revolutionize the way we think about medicine and, indeed, all of biology. With tools like the Nautilus Proteome Analysis Platform that are designed to identify and measure billions of proteins at once, the potential of proteomics may soon finally be realized.
Listen to our podcast to learn how protein biomarkers are enabling a new era in Alzheimer’s research:
MORE ARTICLES